June 2024
Inside This Issue
 Rural Health Clinic Accreditation:
Rural Health Clinic Accreditation:
The June issue of Perspectives contains some new information and announcements, but no new standards, or reinterpretations of existing standards that should cause readers to stop what they are doing to implement key changes.
There is an announcement about a new, CMS deemed, rural health clinic accreditation program that is launching in July that may attract some new rural health clinic (RHC) organizations to Joint Commission. As this accreditation program did not exist previously, there may also be some larger (tailored) organizations with multiple accreditation programs that had their existing rural health clinic reviewed previously under either hospital or ambulatory accreditation standards or other deemed accreditation organization such as The Compliance Team.
Once the new rural health clinic accreditation program becomes operational, you will eventually need to have your RHC reviewed under the new RHC standards. The Perspectives article does not contain guidance on how soon such organizations must undergo a TJC survey using the new deemed status RHC program standards. Perspectives advises such organizations to contact their account executive to discuss options and questions.
 Hospice Standards Changes:
Hospice Standards Changes:
Perspectives also contains an announcement that TJC has edited its hospice standards as of July 1, 2024, to accommodate changes published by CMS. The change basically adds two new professional titles to the glossary; Marriage and Family Therapist (MFT) and Mental Health Counselor (MHC).
These two specialists have also been added to home care standard PC.02.01.05, EP 6 applicable to hospice organizations as staff authorized to participate on the hospice interdisciplinary group. Do take a look at our CMS section of this newsletter as MFT and MHC have also been added to their regulations for rural health clinics and federally qualified health centers.
 Sprinkler Pipe Non-Compliance:
Sprinkler Pipe Non-Compliance:
This month’s Consistent Interpretation column is very brief, but the scoring is huge (53%) due to the difficulty of compliance. The standard/EP in question is LS.02.01.35, EP 4, which prohibits sprinkler pipes from being used to support any other item. Unfortunately, this is a hidden risk as sprinkler pipes are above the suspended ceilings found throughout most organizations. Many hospital staff, contractors, vendors or repair technicians perform work above your suspended ceiling and any one of these individuals can create a compliance problem for your organization while performing their work.
Sprinkler pipes look sturdy, accessible and look like they might support other objects, but they cannot be used to support, drape or touch even a lightweight item. This is a teaching point that is not well understood as many individuals will think their item is just a computer cable, or just a piece of light weight air duct, or it is just touching, not really supporting, but the underlying NFPA requirement prohibits even that minimal support.
So, there are two pervasive problems that that can cause this standard to be scored noncompliant. The first problem is just the vast size and widespread scope of the problem which may already exist but be hidden from view in many locations throughout your organization. The second problem is that any worker, repair vendor, or contractor may create a new noncompliance situation, the very next time they are working above your ceiling. Correcting existing problems and preventing new noncompliance situations can be very time consuming.
An above the ceiling inspection process is recommended to try and find all the vulnerabilities that might already exist in your organization. Telling staff to “go and look” and having staff say, “we are good,” is insufficient. You really want a trackable inventory of rooms, spaces, hallways; a named, assigned inspector for each space and work orders and documentation of corrective actions taken for each deficiency found.
Depending on the size of your organization and the scope of the existing problem, this may take hundreds of hours to complete. In addition, you should consider an “above the ceiling” work permit with guidance on not using sprinkler pipe to support any other materials, and an inspection process after completion and prior to payment to contractors in order to verify compliance with your expectations.
Readers may be wondering why we are belaboring this issue. On most surveys if an organization is cited for this problem all you have to do is fix what the surveyor found and describe the corrective action in your post survey, evidence of standards compliance. However, when the standard falls under a noncompliant Medicare Condition of Participation for physical environment, the problem is subject to onsite review during a follow up survey.
Most of the time the surveyor will take the easy route and look to verify corrective action in the same location where the first surveyor saw the problem. But the surveyor could choose to look elsewhere to verify the CoP is genuinely corrected and not a more pervasive problem. If you only fixed the location that the first surveyor had looked, you remain with some risk, that could cause you to fail your Medicare follow up survey.
If you look at the accreditation process chapter (ACC) of your manual, you should note the decision rule PDA09. You only get two chances to clear your Medicare deficiency survey findings. As the first follow up survey occurs 30-45 days after the full and the second follow up survey occurs only 30-45 days after the first Medicare follow up survey, if you find that you have a widespread problem with sprinkler pipes supporting other materials, you have a very tight timeframe to find and correct what may be a time consuming and expensive issue. Thus, a presurvey, proactive approach is best to find, correct, and prevent this very common problem from existing in your organization.
 Potential Standards Development:
Potential Standards Development:
The last page of Perspectives routinely contains a snapshot of issues TJC is currently exploring for potential standards development. We noticed that the June issue says TJC is exploring potential safe staffing requirements for hospitals and critical access hospitals. This is also an issue some states are exploring for potential state regulations.
It happens to be an issue that TJC has made a run at on at least two occasions over the past 20 plus years. Some readers may remember the first attempt with human resource performance measures that were eventually discontinued. These were eventually replaced by PI.03.01.01, EPs 13 and 14, but neither effort has led to any significant impact on safe staffing. It will be interesting to see what develops out of this latest activity.
Do continue to look at this last page of each month’s Perspectives and potential draft standards that may be developed. TJC usually provides an opportunity to comment on draft standards and as this is a difficult issue to develop standards, comments may be valuable to help prevent another time-consuming project with limited value.
 Sustainability:
Sustainability:
Similar to this month’s issue of Perspectives, EC News contains some informative articles, but nothing that should cause you worry feel the need to stop and change something immediately. The lead article is about sustainability, and while it is somewhat of an advertisement for The Joint Commission’s new sustainability certification, it does summarize efforts by their first sustainability certified organization and discuss steps that can be taken to reduce energy needs and resultant costs.
 Pest Management:
Pest Management:
There is also an article on pest management that recommends what they call an ‘integrated pest management” program and provides a link to a 29-page EPA publication, “Integrated Pest Management in Health Care Facilities” on that issue. The EPA document and the EC News article should be shared with your facilities leadership to compare what the EPA is recommending with our own pest management program.
Metal Detectors:

For those of you who have or are considering metal/weapons detectors at your points of entry, the June issue of EC News contains a summary article on the pros and cons of such systems and provides some implementation suggestions.
Illuminated Exit Signs:
The article we found most informative is on illuminated exit signs, describing the underlying NFPA requirements and Joint Commission’s approach to the requirements. One type of illuminated exit sign is the photoluminescent sign which absorbs light from an appropriate light source and allows the sign to glow in the dark. The NFPA 101-2012 specifically states that such signs should “be continually illuminated while the building is occupied.”

There are specific UL requirements for a reliable light source, and the authority having jurisdiction should determine the adequacy of the light source. These signs need to be visually inspected/documented each month per EC.02.05.07, EP 1.
Battery powered exit signs require testing each month for at least 30 seconds and a 90-minute test at least annually. There are also life safety code chapter requirements for the height of exit sign lettering; internally lit exit sign lettering must be 4 inches and externally lit sign must be at least 6 inches in height.
We would encourage readers to share this article with facilities leadership and to learn what kind of illuminated exit signs you have in which locations, and to verify they are being tested and/or inspected as required.
 Bronchoscopy Environment:
Bronchoscopy Environment:
TJC recently posted a new FAQ on requirements for performing bronchoscopy in a negative pressure environment in accordance with ASHRAE 170-2008. TJC states in their FAQ that organizations can’t just risk assess out of a code requirement.
In the next paragraph TJC states that they “recognize there may be extenuating patient specific circumstances that may preclude a bronchoscopy from being performed in a space specifically designed for that purpose.” As examples they suggest immediacy of the procedure and the inability to move the patient safely. The key action item is that TJC calls for an “established process” to be in place in the event such a situation arises.
Additionally, they advise that the process must address items such as:
- The patient has been evaluated to determine the need to perform the bronchoscopy in a noncontrolled environment.
- The risks have been evaluated of performing the procedure in an alternate location as well as the patient specific risk factors such as risk of airborne communicable disease.
- Mitigation strategies are implemented to minimize risk such as HEPA filtration or scheduling the patient at the end of the day.
At present you can find this FAQ in the New and Featured section of the FAQs, but over time this will migrate to the EC and IC chapters. The FAQ is silent on where to document this process evaluation and organizations are going to want to consider where best to document this, so that it is retrievable if needed. For example, you might want to document the process evaluation and implementation in the medical record, or if you maintain a bedside procedure log on that log, or an infection prevention exceptions log.
 High Alert Medications and Error Prone Abbreviations:
High Alert Medications and Error Prone Abbreviations:
The Institute for Safe Medication Practices has published new lists for 2024 on High Alert Medications and Error Prone Abbreviations. The high alert list provides suggestions for categories of medications which may require additional precautions or safety measures. The list does not suggest enhanced safety strategies but do remember that per Joint Commission’s standard MM.01.01.03, EP 2 the organization is expected to implement a process to enhance safety with high alert medications. This may be double checks, enhanced labeling, unique storage or other strategies to improve safety.
The ISMP list of error prone abbreviations, symbols and dose designations is very extensive, 8 pages in length, and includes many abbreviations we might not have ever considered. The Joint Commission’s prohibited abbreviation list under IM.02.02.01, EP 3 is much more limited, but as you develop organization policies you may want to make additions based on this ISMP list to your prohibited listing. Bear in mind that TJC does survey to your own policies, which may add some survey risk if your list is more extensive, however eliminating the ambiguity of confusing abbreviations may be worth that additional survey risk.
Given that texting of medication orders is now permitted by CMS/accreditors, and the propensity for most people to use many abbreviations in texting, there may be additional value to having a more extensive prohibited abbreviations list in your organization. The ISMP list does provide guidance on how these error prone abbreviations have been mistaken and the potential risks appear very significant.
One interesting example on the ISMP list was the abbreviation “m.” A generation or more ago students entering a healthcare field still learned some basic Latin abbreviations and Roman numerals that were pertinent to medication prescribing, and to them “m” meant “thousand.” Younger healthcare practitioners who grew up texting might more commonly consider “m” an abbreviation for million. We would encourage readers to give this ISMP list a thorough read and consideration.
 ACHC: Joint Ventures Webinar:
ACHC: Joint Ventures Webinar:
ACHC has announced a free webinar planned for June 13 on Hospital-ASC Joint Ventures. This may be valuable to sign up for as we see many organizations entering into such joint ventures and there is a complex regulatory framework from CMS.
CIHQ: Sterile Processing:
The May issue of the CIHQ Journal has an article on Sterile Processing Department-OR collaboration and partnership to

coordinate care and services. The article is written by a member of the consulting firm “Dr. SPD” and recommends open communication between the departments, standard operating procedures, cross training, a culture of mutual respect and collaboration, quality control and audits, embracing technology and fostering a supportive environment. There are some good ideas here to consider given the importance of proper high-level disinfection, sterilization, storage and evaluation of instrument readiness to use.
 Surgical Procedure Consent:
Surgical Procedure Consent:
CMS did something interesting that we have not seen them do previously. On April 1, 2024, they had posted QSO 24-10 discussing additional examinations that might be performed for teaching purposes during a surgical procedure. At some time since that posting, CMS has revised the memo, but did not repost it as a revised QSO with a new date to highlight the change. We would like to thank one of our readers, Lisa C, who noticed the change when she went to re-access the memo on the CMS website. The new content is on page 4 of 5, where CMS has now added:
“A written consent form is required for patients undergoing anesthesia procedures, but patients with the ability to verbally affirm consent for procedures that do not require anesthesia should have their medical record reflect that consent was given. In both instances there is written documentation of consent for any examinations.”
If you downloaded and filed the earlier version of the QSO, you will want to redownload the revised version and verify policy compliance.
Authorized Service Providers:
CMS also posted QSO 24-12 relative to hospice, rural health clinic (RHC) and federally qualified health center providers (FQHC). Similar to the change we discussed in The Joint Commission section of this month’s newsletter for hospice, CMS has now authorized marriage and family therapists or mental health counselors to be participants in the collaborative team approach to providing services to patients in RHCs and FQHCs.
This memo also has some definitional/qualification edits for nurse practitioners, certified nurse midwife, clinical psychologist and clinical social workers, but these technical changes should not have any impact on operations or staffing in RHC or FQHCs.
Consultant Corner
Dear Readers,
Hello and Happy June! We suppose you have noticed by now that our Patton Post looks a just bit different this month. Please join us in welcoming our new-and-improved logo, colors, and style!
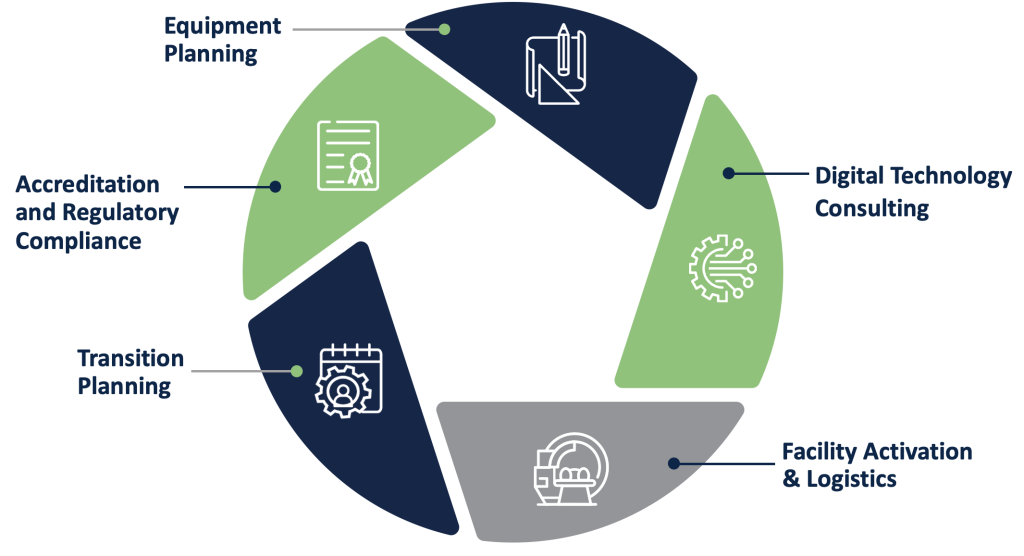
As most of you know, we were acquired by Healthcare Building Solutions (HBS) back in March 2022. Since then, our HBS Family has expanded with the addition of three more sister companies: HTS, Barrins & Associates, and OneEQ.
Each company came with their own unique and individually beautiful style, but together they did not look as if we were one family. With that, HBS created this modern, attractive, and unified look.
We will cherish the memory of our original logo, but we are delighted for this refreshing and long-awaited transformation.
Please check out our range of services we can provide at any stage of your healthcare organization’s journey.
Contact Us to get your survey or project scheduled now! We look forward to hearing from you soon. Thank you!
Thank You,
Jennifer Cowel, RN MHSA
JenCowel@PattonHC.com
Julia Finken, RN, BSN, MBA, CPHQ
julia.finken@hbsinc.com
Kurt Patton, MS RPh
Kurt@PattonHC.com
John Rosing, MHA
JohnRosing@PattonHC.com
HBS. We Bring Buildings to Life.
Equipment Planning
From minor departmental renovations to new replacement facilities, we define requirements, identify challenges, and deliver solutions that help our clients improve healthcare outcomes and operational efficiencies with extensive knowledge of emerging technologies.
Transition Planning
Our Transition Planners generate a clear roadmap for making a new building operational, including “day-in-the-life” planning and workflow mapping to help mitigate risk, minimize redundant operations, and avoid disruption to ensure a friction-free transition to a new facility.
Facility Activation & Logistics
Our Facility Activation experts rely on a team-based process that includes comprehensive logistical plans with clear, user-friendly dashboards that identify, define, and manage building and operational readiness. It’s a process that reduces downtime and helps mitigate risks throughout the crucial go-live period.
Digital Technology Consulting
The need for secure, reliable, and scalable technology has never been greater. Our experts can align your technology investment with specific needs and financial goals.
