March 2022
Inside This Issue
 Before discussing this month’s published changes, we should discuss a more pressing issue and that is the rapid adoption of the evaluation of worker vaccination status by CMS, TJC, and other accreditors. Normally we see a slow roll out and gradual education curve on any new requirement, but the “worker” vaccine requirement seems to have taken off very rapidly.
Before discussing this month’s published changes, we should discuss a more pressing issue and that is the rapid adoption of the evaluation of worker vaccination status by CMS, TJC, and other accreditors. Normally we see a slow roll out and gradual education curve on any new requirement, but the “worker” vaccine requirement seems to have taken off very rapidly.
Survey findings have already been seen and TJC has even issued detailed guidance to its surveyors on what to score and how to score different levels of compliance within the states based on what their specific start dates were per the CMS memos we discussed last month.
Readers may have noticed our use of the term “workers” above instead of the more traditional term “staff.” We did this because the more traditional term “staff” is often associated with employed individuals, and this scope of this vaccine requirement is much broader. It includes employees, individual practitioners with privileges, volunteers, students, contracted staff, and staff who provide offsite patient care, and to staff who provide off site services, but who will sometimes enter the facilities of the Medicare certified organization or otherwise come in contact with coworkers.
Organizing all the data for these disparate groups is not a simple task, and it appears that delayed aggregation of this data may already be leading to some findings that might have been prevented. Complicating the organization of data issue and total compliance levels is the issue of medical and religious exemptions.
If the organization has completed the decision-making process on the exemption request, in accordance with Federal laws, and determined it to be valid, these workers and the organization are essentially compliant with the Federal mandate. However, if the exemption decision is still pending, the worker falls in the rate calculation as unvaccinated.
We are also hearing of issues arising from practitioners with privileges who may not be employees or contactors, but are providing patient care services in person at the healthcare organization. Such individuals must also be vaccinated and included in the calculation analysis.
Questions are already arising about what to do if the practitioner with privileges refuses vaccination. The perfunctory response we are hearing from the authorities is just to terminate their privileges, but such action is not to be taken lightly. Actions taken against privileges are reportable to the National Practitioner Data Bank and any actions taken must be done in accordance with the medical staff bylaws, rules and regulations and policies.
Bylaws developed in accordance with MS.01.01.01 have multiple reference points in EPs 4, 5, 6,1 1, 28, 30, 31, 32, 33, and 34 which may be helpful to you in designing your process to manage unvaccinated practitioners with privileges. Employment contracts that may be a part of the process might be easier to manage quickly than would privilege removal.
We would also advise consulting with your hospital attorneys in designing any process for managing such issues. Unfortunately, while you are managing through this issue, these individuals would be considered unvaccinated and calculated as such in your non-compliance percentage.
TJC has developed what might be considered policy expectations for implementation of your vaccine program including:
- Your process for tracking and securely documenting vaccination status for workers
- Your process for tracking and securely documenting vaccination status of workers who have taken boosters
- Your process for staff to request an exemption to the requirements
- Your process for securely documenting information provided by workers in requesting an approved exemption in accordance with Federal law
- Your process for verifying that a medical exemption request is based on recognized clinical contraindications; N.B. Surveyors will not be second guessing individual exemptions, they will only validate that you have developed a scientific process; your process should ensure that requests come from licensed practitioners, acting within their authorized scope of practice
- Your process for ensuring the implementation of additional precautions designed to mitigate the transmission of Covid for staff who are not fully vaccinated
- Your process for tracking and securing PHI documentation for those whose vaccination must be temporarily delayed due to either having received monoclonal antibodies or convalescent plasma
TJC has developed three (3) levels for scoring noncompliance with the vaccination requirement including immediate threat to health and safety (ITHS), condition level, and standard level. The immediate threat level would be considered if the noncompliant percentage of workers is 40% or greater, or any amount less than 100% coupled with observations of noncompliant infection control practices, or one or more the aforementioned policy/process requirements were not developed or implemented.
As is usually done prior to implementing any ITHS level decision, the surveyors would have to discuss the plan with their central office. The condition level finding would be issued if 21-39% of staff are unvaccinated or anything less than 100% combined with portions of the required policies/processes that are undeveloped. Lastly the standard level scoring would be issued is 10-20% of staff are not vaccinated or anything less than 100% and one or more portions of the required policies/processes are not developed or implemented.
TJC and CMS may lower the citation levels if there have been mitigating circumstances such as a lack of access to vaccine or there has been very aggressive actions taken, but success has not yet been achieved. Unfortunately, these are subjective considerations, but if you are less than 100% compliant do try to articulate the degree of effort taken to be successful.
As you proceed with your planning on this issue, do take a look at the now 32 “new” standards FAQs that TJC has posted to their website on this subject. They are all identifiable at this time as “new”, but may become more difficult to locate when the “new” subject header is removed.

2021 End of Year Analysis:
This month’s issue of Perspectives provides an end-of-year 2021 analysis of sentinel events reported to or identified by TJC. You will first notice a large spike in reporting volume between 2020 and 2021 with almost 400 more sentinel events than in 2020. The year 2020 had been a slight decrease from 2019, but as you may remember all too well, 2020 was a year full of epidemic related Covid issues and high patient census which may have reduced the ability to report or identify sentinel events.
Perhaps in 2021 organizations were able to get back to more normal identification and analysis processes. The largest category of sentinel events is care management issues, with patient falls being a large component of the category. We also noted there were 79 suicide events reported last year, very similar to 2020 when there were 81.
TJC provided a link to their web-based sentinel event data and this further breaks down the suicide events into 42 occurring offsite within 72 hours of discharge and 36 occurring in the inpatient sector. There was one suicide reported in the ED setting. We do recommend following the link to the web data to look at all the categories of sentinel events reported or analyzed to help identify potential vulnerabilities at your own organization or perhaps opportunities to proactively redesign a high-risk process.
Hospice Changes:
Our readers with hospice programs should note that this month’s Perspectives has additional standards changes for hospice programs. There are two new terms defined in the glossary, pseudo-patient and simulation. A pseudo-patient is a trained individual or computer-based mannequin able to perform role playing and verbally interact with staff during training. A simulation is training and assessment activities that mimic the home care environment including environmental distractions and constraints that staff might have in the real-world environment.
The first standard change is in HR.01.03.01, EP 24 relative to staff supervision has been modified so that when supervisory staff observe a hospice aide with deficient skills during an onsite observation, there should now be a follow up competency evaluation on the aide to ensure that the aide has acquired the skills needed. Although not stated this follow up competency assessment would of course be after some refresher training and guidance.
HR.01.06.01, EP 9 is also modified so that when you are assessing competence of an aide’s ability to interact with a patient or pseudo-patient, you evaluate communication skills, including the ability to read, write and verbally report clinical information and evaluate the aide’s ability to read and record vital signs including temperature, pulse and respiration.
Suicide Prevention and Screening: 
This month’s Consistent Interpretation column discusses the National Patient Safety Goal on suicide prevention and more specifically the screening process. Looking at the Guidance/Interpretation section is a helpful refresher on essential features as important requirements have been distributed to Perspectives articles, standard FAQs and the Suicide Prevention Portal. For example, this article reminds readers that:
- Validated screening tools cannot be modified
- The PHQ-2 is not perceived as a validated screening tool
- The PHQ -9, using only question 9 is not perceived as a validated screening tool
- If you screen everyone who arrives at your facility including those not seeking or in need of behavioral health services, you can use any screening method you wish; but a validated tool must be used for behavioral health patients
- Validated tools must be used for those age 12 and above seeking behavioral health services; below age 12 you can determine how you will screen these individuals
The last element of guidance we noted is perhaps the most important from a patient care perspective and that was their comment: “If a patient triages as a high risk or imminent risk using a validated screening tool, one-to-one continuous observation is expected until the full assessment is completed to determine the level of risk, if the patient is housed in an area that contains ligature and or other safety risks.”
We found the second half of the sentence somewhat odd requiring one-to-one, only if the environment has risk. We would encourage readers to use one-to-one until a full assessment can be conducted, regardless of the perceived safety of the environment.
Each year more and more devices or fixtures are being identified as potentially hazardous because an ingenious patient found a creative but dangerous way to use that device.
Prevention of Surgical Fires:
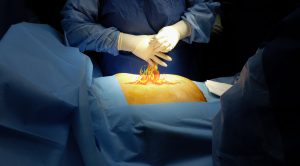
The lead article in this month’s EC News discusses an important subject, the prevention of surgical fires. The article provides a good foundation for learning fire basics by explaining the role fuel, ignition source and an oxidizer, surgical drapes, gauze, alcohol containing skin preparations, and oxygen may play in a fire situation.
They also note that even endotracheal tubes can serve as a fuel source and they do account for a significant portion of OR fires. Fortunately, there are now FDA approved ET tubes that are considered laser resistant.
The article does mention the existing NFPA 99-2012 language that requires any solution-soaked material to be removed from the operating room prior to draping or using electrosurgery, cautery or a laser.
They do not specifically reference the agreed upon reinterpretation of that guidance, but readers should take a look at the Perspective’s Consistent Interpretation column published in February 2021 that provides guidance that it is acceptable to only remove those solution-soaked materials from the proximity of the patient, not removed from the operating room itself.
The article is a useful refresher on fire safety for operating room staff and we want to remind readers that there is a new EP 7 in EC.02.03.03 that takes effect in July 2022. The EP requires an announced or unannounced annual fire drill in anesthetizing locations if your organization uses flammable liquids, germicides or antiseptics in conjunction with electrosurgery, cautery, lasers or other ignition sources.
Protecting Patients at Risk for Suicide:
EC News also has a useful high-level summary of requirements for assessing the environment to help protect patients at risk for suicide. The entire body of information published in the last few years on this issue has been voluminous, with multiple Perspectives articles, many standards FAQs, and the content in the suicide prevention portal on the Joint Commission website. The article is a helpful revisit on this important content and given the continued frequency of identified safety goal noncompliance and more importantly the continued frequency of suicide sentinel events, revisiting the issue of the physical environment would be valuable.
Surveying for Vaccine Compliance: 
There was one new QSO memo published in the past month, QSO-22-12 dated February 9, 2022. When the Covid-19 vaccine mandate was being implemented there was discussion in some states about not surveying for compliance on this issue. In this QSO CMS is basically reminding the states that they are contracted to survey all conditions of participation and requirements. CMS intimates that provider certifications and state funding may be jeopardized if there is a failure to conduct complete surveys.
Medication Errors:
The Institute for Safe Medication Practices authored a summary review of
medication errors identified during the prior year, 2021. This summary was published in Pharmacy Practice News and is available through their website at PharmacyPracticeNews.com

The article provides seven (7) tables of information that will be useful to review to help prevent similar types of errors from occurring in your own organization. The tables, each with multiple different types of events are:
- Safety issues related to labeling, packaging, and nomenclature
- Safety issues associated with order communication
- Problems involving drug information, patient information, patient and staff education
- Safety issues related to medical devices and equipment
- Problems associated with Covid-19
- Other discussion items
- ISMPs targeted medication safety practices for hospitals
We encourage readers to download this article and discuss it within an appropriate forum in your hospital to identify any gaps or improvement opportunities you spot when comparing your current processes against this summary.
Consultant Corner
Dear Readers,
We are here for you before, during, and after survey to assist you and your healthcare organization in accreditation and compliance.
We help simplify the many challenges, so you can deliver safe and compliant patient care.
Jennifer Cowel, RN MHSA
JenCowel@PattonHC.com
Kurt Patton, MS RPh
Kurt@PattonHC.com
John Rosing, MHA
JohnRosing@PattonHC.com
Mary Cesare-Murphy, PhD
MCM@PattonHC.com
