March 2025
Inside This Issue
ALC, BHC, and NCC Adverse Decisions:
 TJC announced in their March issue of Perspectives a new APR and two new decision rules that only apply to assisted living, behavioral health and nursing homes, but it is a major departure from their methodical and slow process for adverse accreditation decisions. Effective at the end of this month a new immediate threat APR.09.04.01, EP 2 will be added that states: “As determined by the sole discretion of The Joint Commission, the organization provides care, treatment or services and/or a safe environment that meets minimal accreditation requirements of quality and or safety of individuals served and or staff.”
TJC announced in their March issue of Perspectives a new APR and two new decision rules that only apply to assisted living, behavioral health and nursing homes, but it is a major departure from their methodical and slow process for adverse accreditation decisions. Effective at the end of this month a new immediate threat APR.09.04.01, EP 2 will be added that states: “As determined by the sole discretion of The Joint Commission, the organization provides care, treatment or services and/or a safe environment that meets minimal accreditation requirements of quality and or safety of individuals served and or staff.”
This APR requirement is accompanied by two new decision rules, DA13, denial of accreditation for initial accreditation and DA08, denial of accreditation for organizations that are going through a reaccreditation survey. Assumedly this would not be applied often or without some internal deliberation, but the swiftness of the process is a significant departure from today’s preliminary denial of accreditation process and the opportunity for hearings or appeals.
New IC Chapter for Laboratories:
 Perspectives announced a revised IC chapter for laboratories that takes effect July 1, 2025. The revised chapter is posted to the prepublication section of their website, and the posting indicates it was posted February 20, 2025. Thus, you have four and a half months to get ready rather than the usual 6-month advance notice.
Perspectives announced a revised IC chapter for laboratories that takes effect July 1, 2025. The revised chapter is posted to the prepublication section of their website, and the posting indicates it was posted February 20, 2025. Thus, you have four and a half months to get ready rather than the usual 6-month advance notice.
Posted with the revised standards is what they call a reference guide that details what requirements have moved from another standard/EP reference and what requirements had no previous reference and appear to actually be new requirements. There are three (3) standard references that identify NA, or not applicable in the old standard column on the reference guide and this effects four (4) elements of performance. These entirely new requirements are IC.04.01.01, EP 3, IC.06.01.01, EP 1 and IC.07.01.01, EPs 1 and 2.
We would suggest downloading the revised chapter and reference guide, now, while it is available on the prepublication site. Be sure to note the elements of performance that describe documentation required as you likely will need to develop some new policies and documentation streams to create your evidence of compliance.
The Perspectives article also described a new IC Assessment Tool that “details practices and structures to meet the IC requirements.” TJC indicates that this will be posted to the organization’s extranet website by March 1. As TJC did not explicitly state where it has been placed on the extranet site, or if this is a laboratory specific tool, we initiated a search to try and find it. We did not find a laboratory specific tool, but we did find an Excel spreadsheet for conducting risk assessments for potential infection hazards. This was accessed via the extranet via a link to Patient Safety Topics on infection prevention. We are not sure if this is the tool they were describing, however it looks useful.
Hospice Life Safety Code Surveyor:
 Perspectives also announced that TJC is adding a life safety code surveyor to all hospice deemed status surveys effective immediately. There is a new March edition of the customer Survey Activity Guide, and this guide describes the tasks assigned to the life safety code surveyor and provides a template agenda for this additional surveyor. These life safety code surveyors have been a regular participant on hospital surveys for many years now and they have great expertise on building code construction requirements and NFPA manuals.
Perspectives also announced that TJC is adding a life safety code surveyor to all hospice deemed status surveys effective immediately. There is a new March edition of the customer Survey Activity Guide, and this guide describes the tasks assigned to the life safety code surveyor and provides a template agenda for this additional surveyor. These life safety code surveyors have been a regular participant on hospital surveys for many years now and they have great expertise on building code construction requirements and NFPA manuals.
When we review TJC hospital survey reports the EC and LS chapters alone often contribute as many findings to the total report as do all the clinical standards. This change may have a very significant impact on deemed status hospice surveys that will require both study and preparation, particularly if you have not had a state surveyor focused on life safety code issues in recent years.
Due to the risk and short notice, we encourage you have an expert review your compliance with the EC/LS expectations. Patton has an experienced and skillful bench of EC/LS/EM experts, please reach out to us at ExpertAdvice@pattonhc.com
Multifactor Authentication:
 Perspectives describes an upgraded authentication process to log onto The Joint Commission connect website. They indicate this will enhance security, but require resetting a password and establishing a connection, email, text, or phone call for multifactor authentication.
Perspectives describes an upgraded authentication process to log onto The Joint Commission connect website. They indicate this will enhance security, but require resetting a password and establishing a connection, email, text, or phone call for multifactor authentication.
If you were concerned about access to your confidential documents on the extranet, this will enhance security. If you find multifactor authentication a tedious, repetitive delay, the Perspectives announcement did not mention an opt out process.
Orientation of New Staff:
 This month’s Consistent Interpretation column discusses HR.01.04.01, EP1 which requires orientation of new staff to key safety content before providing care, treatment or services. This EP does have a D for documentation. Scoring last year on this issue was minimal, with only 2% of hospitals being scored noncompliant.
This month’s Consistent Interpretation column discusses HR.01.04.01, EP1 which requires orientation of new staff to key safety content before providing care, treatment or services. This EP does have a D for documentation. Scoring last year on this issue was minimal, with only 2% of hospitals being scored noncompliant.
The guidance to surveyors section advises them to score a lack of staff awareness on how to respond to an environment of care incident at EC.03.01.01, EP 2, so there may be more total scoring on this issue than just that 2% figure attributable to the HR reference only. The article also provides links to two of Joint Commission’s standards FAQs, and the link to the FAQ on competency vs orientation has some additional suggested orientation topics that many organizations choose to include.
While scoring on this standard/EP has not been huge, it may be a good time to verify you have these important data elements mentioned in your orientation materials and that you have verification that staff attended this orientation session. As consultants we often find an important content element that is not mentioned in any documentation, or an inability to find evidence that an employee ever attended the session where this content was discussed.
Clinical Fires:
 This month’s lead article discusses clinical fires and TJC provides some very informative examples of clinical fires that impacted organizations during 2024:
This month’s lead article discusses clinical fires and TJC provides some very informative examples of clinical fires that impacted organizations during 2024:
- Fire caused by high flow oxygen humidifier
- Fire caused by a wireless speaker lithium battery pack while being charged
- OR table fire caused by a lithium battery pack in the table
The article summarizes some of the impacts of these fires, including damage to 25,000 square feet of hospital space due to water flow from sprinklers used to suppress the wireless speaker fire.
While we sometimes are encouraged by the thought that: “this has not happened at our organization,” these examples should give everyone pause, because it can. TJC reminds readers that standard EC.02.03.03, EP 7 requires an annual OR specific fire drill, and they have an informative standards FAQ on their website about which types of fire extinguishers to use in surgical areas and advice to consider sterile water rather than a water mist fire extinguisher during a surgical procedure.
We suggest that readers share this article with OR and facilities leadership and use it to help educate and plan for this year’s OR fire drill. We found the examples of fires and damage caused by lithium-ion batteries particularly helpful. We have seen many examples of phones, radios, speakers and other personal music devices in empty offices charging and this may be a hazard you want to mitigate.
Preventing Falls in the Physical Environment:
EC News has a good refresher article on preventing falls that the summarized national estimates of the total number of falls in all US hospitals is somewhere between 700,000-1,000,000 per year. They also advise that falls is their number one most frequently reported sentinel event with 672 falls reported in the database during 2023. This included 26 fatalities, 56 permanent harm events, and 538 severe harm events. EC News also reminds us that falls don’t just happen to patients, falls from slipping can happen to staff and visitors as well.
 TJC provides 16 suggestions for improvements that may help to reduce the risk of falls including:
TJC provides 16 suggestions for improvements that may help to reduce the risk of falls including:
- Examine floors for wear or damage that might lead to a tripping hazard
- Organize patient rooms so that patients can reach personal items
- Repair broken nurse call lights or cords and implement no pass zone policies
- Replace burned out or flickering lightbulbs
- Eliminate unused equipment including canes and walkers from patient rooms
- Construct floors using non-slip surfaces in toilet or shower areas and use no skid wax
- Repair or replace broken wheel locks on beds, wheelchairs or stretchers, and ensure locks are in the locked position
- Ensure corridors are free of clutter
- Don’t block corridors with equipment, or power cords that cross the floor
- During wet weather keep corridors and rooms clean and dry
- Use caution wet floors signs during mopping
- Clean up spills immediately
- When wet processes are performed use platforms, mats or other dry areas
- Avoid construction dust or other contamination in hallways
- Encourage employees to wear appropriate nonskid footwear
- Educate and train on fall prevention initiatives
Emergency Lighting Q&A:
 The March issue of EC News has a very useful article on emergency lighting requirements and testing expectations. Testing is described in EC.02.05.07, EPs 1 and 2. EP 1 requires a monthly test of emergency lighting and exit signs required for egress, and task lighting for a minimum duration of 30 seconds. EP 2 requires a 90-minute test of the same, every 12 months. When you perform your 90-minute test, you don’t have to perform the 30 second test that month.
The March issue of EC News has a very useful article on emergency lighting requirements and testing expectations. Testing is described in EC.02.05.07, EPs 1 and 2. EP 1 requires a monthly test of emergency lighting and exit signs required for egress, and task lighting for a minimum duration of 30 seconds. EP 2 requires a 90-minute test of the same, every 12 months. When you perform your 90-minute test, you don’t have to perform the 30 second test that month.
In addition, the life safety code chapter has three (3) elements of performance in LS.02.01.20, EPs 38, 39 and 40, with EPs 38 and 39 establishing requirements for egress illumination and exit illumination and EP 40 establishing requirements for exit sign placement and size. This article would be a good discussion document to begin a review of internal documentation of testing and verification of adequacy of illumination and placement.
Protection from Fire:
 The last article in EC News discusses occupancy types and protecting patients from fire. One confusing issue that arises is: What exactly is the requirement for ambulatory occupancies in hospitals?
The last article in EC News discusses occupancy types and protecting patients from fire. One confusing issue that arises is: What exactly is the requirement for ambulatory occupancies in hospitals?
This article has a boxed advisory that CMS has established more stringent requirements for ambulatory surgery centers and outpatient surgery centers of hospitals that require the outpatient location to meet at least the ambulatory occupancy requirements, even if only one patient is mostly incapable of self-preservation, not the four (4) or more that are described in NFPA. This article also contains a link to another of the JCR tools for self-evaluation of fire prevention and control.
 Natural Disasters and Evacuations:
Natural Disasters and Evacuations:
The February issue of the new Joint Commission publication, EM Leader came out after we had published our February Patton Post newsletter. As you might anticipate, there are some articles relative to wildfires, given what just happened in California. The last article in this month’s issue, quoting from an article originally published in the American Journal of Public Health 2023, indicates that wildfires have accounted for 18.4% of hospital evacuations since 2001. This article also contains a link to a JCR tool created to help organizations prepare for wildfire situations.
EM Leader has another article with links to an AHRQ Hospital Evacuation Decision Guide. This then provides additional links to a decision guide to help determine when a hospital should evacuate given the nature of the pending disaster. The AHRQ material appears to be from 2018, but given what has recently happened, it certainly seems pertinent to today’s emergency management planning.

ACHC: Physical Environment Management Plans:
On February 11th, ACHC posted a brief but helpful blog discussion: Bridging the Gap: Understanding the Interconnection Between the Physical Environment and Life Safety Code Standards for Hospitals. ACHC has requirements for management plans in their Physical Environment chapter. The plans they require should not surprise our readers:
- Building Safety
- Building Security
- Hazardous Materials
- Fire Safety
- Medical Equipment
- Utility Systems
The blog then includes advice for creating a fire safety management plan starting with two (2) building blocks, combining requirements from their Physical environment chapter for fire safety and requirements from their life safety code chapter for means of egress + fire alarm systems + fire suppression systems + fire safety systems.
ACHC then suggests a typical management plan outline including:
- Purpose of the Policy
- Scope of the Policy
- Policy Statement or Description
- Essential content expectations from the PE and LS chapters
- Evaluation of effectiveness, PI and monitoring activities
The content headers we bold coded could remain consistent across your management plans, and the essential content pieces would be derived from the standards for Safety, Security, Hazardous materials, etc. As many people sometimes don’t know where to start or how to start a management plan, this seemed like a simple conceptual framework to use.

DNV: Compliance Automation:
DNV posted their HealthHub newsletter to LinkedIn on February 27th, How to Leverage New Tools for Compliance Automation. Here you can access this newsletter article and subscribe to future publications.
CIHQ: Standards, Policies, and Survey Activity Guide:
We did not see the CIHQ newsletter posted as we were writing ours, but we did find a page on their website that allowed us to download their standards, accreditation policies, and survey activity guide: https://cihq.org/acc-default-hospitals.asp. As you might imagine, downloading their entire standards manual is a lengthy process.
NIOSH: Hazardous Medications:
 The National Institute of Occupational Safety and Health, or NIOSH a division of the CDC has published an updated list of hazardous medications dated 2024, Hazardous Drug Exposures in Healthcare. The link will direct you to a landing page where you can access the recently published 2024 list, as well as the 2023 document for Managing Hazardous Drug Exposures, and another 2023 publication on how NIOSH identifies hazardous drugs – you will want all three (3).
The National Institute of Occupational Safety and Health, or NIOSH a division of the CDC has published an updated list of hazardous medications dated 2024, Hazardous Drug Exposures in Healthcare. The link will direct you to a landing page where you can access the recently published 2024 list, as well as the 2023 document for Managing Hazardous Drug Exposures, and another 2023 publication on how NIOSH identifies hazardous drugs – you will want all three (3).
The last official list was published back in 2016, when it had been on an update schedule about every two (2) years. The forward in the new 2024 document does contain an important warning stating that the new publication’s list of hazardous medication is “not all inclusive.” While they did add 25 new drugs to the list, the drugs added were approved by the FDA or received new warnings from the FDA during the period January 2014 – December 2015. Drugs receiving FDA approval or new warnings during and after 2016 are not yet part of this listing.
Hospitals will still have to evaluate drugs they may be using for possible inclusion on your hospital specific list of hazardous medications. That third publication mentioned above may be helpful in screening which drugs you use that should be added to your list. As a reminder USP Chapter <800> does include a ”must” requirement to have a facility specific list of hazardous medications. TJC’s MM.01.01.03 also requires a hospital to identify the high alert and hazardous medications that are used.
After you have solidified your hospitals list of hazardous medications in use, you will want to re-review the 2023 NIOSH publication on Managing Hazardous Drug Exposures. This document suggests an “exposure assessment”, followed by a “risk assessment” evaluating the different hazards, the probability of exposure and the severity of health effects. The next step is then a risk management plan to protect workers from the effects of hazardous medications.
While this may seem like a huge new burden, to some extent the work you were already doing to implement USP Chapter <800> is helpful because you were doing that analysis, knowing that the 2016 NIOSH Hazardous Drug List was out of date, and therefore evaluating other products you were already using for potential hazard identification. But, to the extent that the analysis for USP Chapter <800> was lagging, you will want to finalize your analysis, as this may be on more surveyors’ radar than previously.
NCC Restraints and Psychotropic Medications:
On March 10, 2025, CMS posted QSO 25-14-NH. This is for the nursing home industry and had been initially posted 1/16/25 as QSO-25-12 NH as an advanced copy. It appears the key modification is to minimally delay the implementation from March 24, 2025, to April 28, 2025. This regulatory memo only affects the long-term care industry, but as we suggested in January, if time permits hospitals readers may want to read the memo’s guidance on restraints and psychotropic medications as they reflect current CMS thinking that may be incorporated into hospital guidance at a later time.
CONSULTANT CORNER
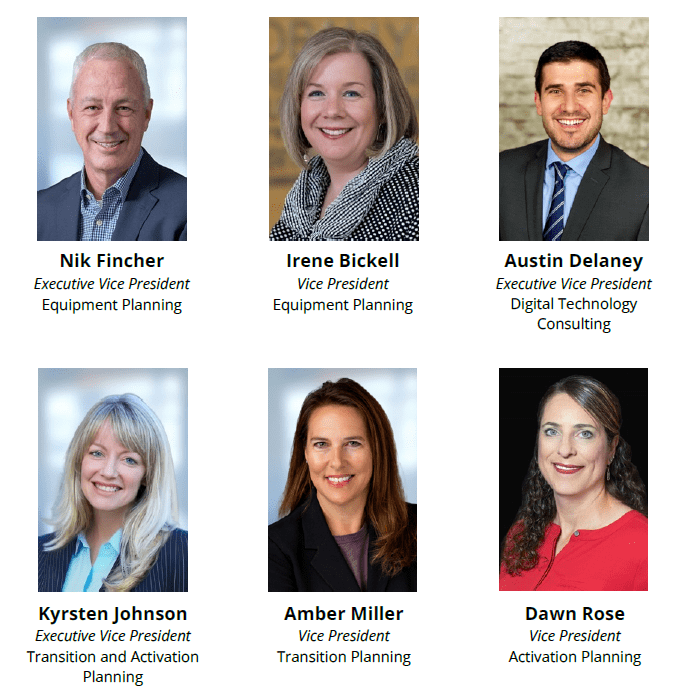
As you may know, Patton joined HBS in 2022, and this week we are celebrating our 3 Year Anniversary! Since
then, HBS has grown and evolved, becoming a dynamic family of companies dedicated to providing comprehensive solutions in healthcare, science, and technology. Through this transformation, we have expanded our expertise, strengthened our capabilities, and have continued to deliver the high-quality services you rely on.
Each of our business unit leaders brings deep industry knowledge, a commitment to excellence, and a passion for helping our clients navigate complex challenges. We would like to introduce you to the other incredible leaders of HBS driving your organization’s success!
Thank You,
Jennifer Cowel, RN MHSA
JenCowel@PattonHC.com
Julia Finken, RN, BSN, MBA, CPHQ
julia.finken@hbsinc.com
Kurt Patton, MS RPh
Kurt@PattonHC.com
John Rosing, MHA
JohnRosing@PattonHC.com