May 2021
Inside This Issue
 Top 10 High & Moderate Risk Findings for 2020:
Top 10 High & Moderate Risk Findings for 2020:
This month we will not be breaking our discussion into high or lower priorities since Perspectives has some good information about scoring practices experienced in 2020. There are no immediate action requirements as a result of new standards or revised interpretations of existing standards.
Provided is a detailed look into scoring patterns identified last year (2020) for all accreditation programs. Due to the pandemic, total survey volume was less than in prior years. This data is presented very differently than in the past where the frequency of scoring a particular standard identified the top 10 issues.
This year the presentation format is more granular and identifies specific elements of performance where surveyors used the TJC SAFER™ Matrix to identify the particular finding as high risk or moderate risk. Thus, a low risk and widespread issue that is scored in 80% of the organizations surveyed will not display in this data.
As you might expect, in the hospital accreditation program the issue that is most often scored with high or moderate risk is related to suicide safety. The first element of performance is NPSG.15.01.01, EP 1 which requires the suicide risk assessment of the physical environment. This was identified at a high-risk level in 99 hospital surveys and at a moderate risk level in another 107 hospital surveys.
Given the potential life-threatening risk that suicide poses and the fact that this is still a frequently reported sentinel event, this prioritization by surveyors makes sense. One of the flaws we often see with environmental risk assessments is a failure to document all observed and theoretical risks. Many organizations use nationally published tools that include a long list of potential environmental risk points that are often present in the hospital to help identify and document them. But if the tool fails to include all of the risks present in the hospital’s actual environment, staff often forget to add a line and list the newfound risk unique to their hospital.
These tools are a great start, but remember if you find an additional item that could be a ligature hazard, you need to add it to the risk assessment tool. For example, it is not common to have a basketball hoop in a gym area and such a potential hazard is not typically going to be on a national environmental risk assessment tool. But if you have one that is used by psychiatric patients you need to document that you recognize the risk and have mitigated that risk through staff supervision.
The second element of performance scored very often in the high and moderate risk category is IC.02.02.01, EP 2, which establishes requirements for high level disinfection and sterilization. As you might assume, any defects in these processes are high risk because there may be transmission of infection. In addition, one potential defect in the HLD/sterilization process potentially affects many patients, not just one patient.
The third high risk EP is IC.02.01.01, EP 1, which is a very basic requirement to implement your infection prevention practices. We refer to this EP as a catch all, where just about any defect that could facilitate the spread of infection can be scored. This can be a wide range of issues from adhesive residue on medical equipment to, dust in patient care areas, to improper equipment cleaning. Given the lesser risk in this EP as compared to the prior issue about HLD and sterilization, the vast majority of these findings were scored in the moderate orange category rather than the highest risk in red.
The fourth most frequently scored EP is MM.06.01.01, EP 3, which somewhat surprised us. The standard has not made the previously published top ten lists, and in our review of survey reports this was never a frequently seen requirement for improvement. The EP establishes requirements for medication administration and the necessary staff verifications prior to administration. We then noted the third column TJC published in this article titled Keywords/Topics. These are searchable keywords surveyors can use to help them find where to score a particular issue.
Take a look at a second article they published in this May issue of Perspectives on page 25 discussing “artificial intelligence.” This searchable keyword methodology helps a surveyor find where to score a particular issue and helps to standardize placement of findings. This keyword logic may be helpful at your own organization to assist staff in correct identification of a standard and EP to score for an issue they see. We have a similar keyword logic built into our consultation survey documentation tool that assists our consultants in correct placement of findings also.
One of the keywords they have included from this element of performance is “titration rates.” As we have all seen for maybe the last five years, medication titration adjustments and documentation have been one of the more frequently scored issues on survey. Previously we have seen a failure to adhere to the prescribed titration adjustment methodology scored under PC.02.01.03 for a failure to adhere to orders as prescribed. We presume that as standardization proceeds with their “artificial intelligence” scoring model, this is now the preferred placement for titration adjustment issues. This particular issue looks to be pretty evenly split between high and moderate risk levels.
The fifth most frequently scored EP is EC.02.05.01, EP 15 deals with air pressure relationships in critical spaces such as operating rooms, sterile compounding, or central sterile supply areas. This has been a frequently cited issue for many years and also one with substantial risk due to the fact that the protective air pressure relationship, positive or negative, is not working as required for the tasks performed in that space. The 2020 scoring data is also evenly split between high risk and moderate risk.
We see multiple flaws with this issue on consultations, one of which is failure to give staff a tool or method to easily detect air pressure deviations. Many settings still don’t have a meter, an alarm or even a ball in the wall device to identify the correct air pressure relationship. Sadly, the second most frequent defect we see is a failure to take immediate action when air pressure relationships are known to be incorrect. Sometimes staff turn off the annoying alarm and keep working without fixing the root cause issue.
The sixth most frequently scored EP is EC.02.06.01, EP 1. This has historically been another “catch all” EP where just about any defect in the environment from torn furniture to suicide hazards have been scored. The keywords TJC has now built into their survey report tool now include safe environment, interior spaces, dirty ceiling tiles, porous surfaces and sterile compounding area. Given the more intense focus on sterile compounding areas, this may be leading to some of these findings. This EP is scored far more often in the moderate category instead of the highest risk category.
The seventh most frequently scored EP is EC.02.02.01, EP 5 which requires the organization to minimize risks associated with hazardous chemicals. We frequently refer to this EP as the eyewash EP where a lack of access to an eyewash, an improper eyewash, or failure to test an eyewash could potentially be scored. Bear in mind that far more than just eyewash issues can be scored here, such as failure to provide or use appropriate PPE for handling hazardous chemicals. This is scored about twice as often in the red, high risk category rather than the moderate orange category.
The eighth most frequently scored EP was NPSG.15.01.01, EP 5. EP 5 was one of the new requirements added a couple of years ago which requires adherence to written policies and procedures in the care of patients at risk for suicide. TJC states that at a minimum these policies and procedures should address training and competence of staff, guidelines for reassessment, and constant monitoring patients who are at high risk for suicide. Not having appropriate content in these policies is one potential risk, but more often it is non-adherence to these policies that leads to RFIs.
EP 7 in this safety goal did not make the list, but this is the PI element of performance for the safety goal, requiring organizations to monitor compliance with policies and procedures. Doing thorough PI on these processes is really the key to preventing TJC surveyors from identifying gaps in adherence to safety measures designed to protect patients at risk for suicide. We have noted on consultation surveys that organizations establish timeframes and use of a particular tool for assessment whereas reassessments are sometimes missed, or the required tool is not used. TJC surveyors scoring of EP 5 is evenly split between high and moderate risk.
The ninth most frequently scored EP was again from NPSG.15.01.01, EP 4. This EP requires documentation of the overall risk for suicide and the plan to mitigate that risk. This was scored by TJC in the red, high risk category more than twice as often as in the moderate. This makes sense as it indicates the hospital has identified suicide risk but failed to take the necessary action to mitigate that risk.
The key to success would appear to be not letting budgets or staffing shortages get in the way of ensuring that each patient identified to be at high risk to have the required 1:1 supervision. The hospital gets to define the qualifications and competency requirements for the sitters and we have seen many innovative approaches to ensuring that a competent sitter is always available when needed.
The tenth most frequently scored EP is IC.02.02.01, EP 4 which establishes infection prevention requirements for safe storage of medical equipment, devices, and supplies. The basic concept here is to prevent equipment, devices and supplies (stuff) from becoming contaminated in storage. Thus clean “stuff” is stored in the clean utility room and it is protected from sink splashes, dust, or employee contamination.
We noted TJC included the term “ultrasound probes” in their keyword section. Given the detailed high-level disinfection work that staff perform for intracavitary probes this means keeping the now clean probe clean until it is used again, which may require a cover or cabinet to protect it. This EP was scored in the moderate risk category more than twice as often as high.
 Interoperability Standard Revision:
Interoperability Standard Revision:
The new standard TJC announced in last month’s issue of Perspectives on interoperability has already been revised. This is likely due to continuing “feedback” from CMS. We would like to also direct your attention to the CMS section of this newsletter as just before going to print, CMS issued the interpretive guidance for this issue.
The TJC change is noted in IM.02.02.07, EP 5 which discusses notifications the hospital must send to aftercare providers. The content changes are minimal but perhaps the breadth and scope of what surveyors will be examining may be more detailed. In last month’s wording, your EMR system needed to send notifications to post-acute service providers “as applicable” and now the requirement says to “all applicable.”
There is a second change to send notifications to other medical providers and the wording change is the addition of the phrase “as well as any of the following” and then it includes the same list of primary care practitioners, primary care group or practice, and other practitioners or practice groups the patient identifies as primarily responsible for their care.
So, if your patient has a PCP and a cardiologist or other specialist the patient identifies as primarily responsible for their care, you would want to ensure that both providers receive the aftercare notice.
New Speak Up Video:
TJC announced a new Speak Up video they have developed for new parents. It addresses four clinical issues: hypertension and preeclampsia, hemorrhage, infection, and depression. This caught our attention because of the hemorrhage and preeclampsia content.
The new maternal safety standards PC.06.01.01, EP 7 and PC.06.01.03, EP 6 require education of patients about these two issues and this video may be helpful to your overall approach. We do have a preference for printed materials that a patient can refer to, but this video might be a valuable component of your patient education initiative.
 Insulin Pen Sharing, Glucometer Cleaning, Lancet / Lancet Holder Sharing:
Insulin Pen Sharing, Glucometer Cleaning, Lancet / Lancet Holder Sharing:
At times we discuss the Consistent Interpretation column because it adds clarity to understanding an existing or newly published requirement, or the article speaks to a standard that is cited frequently. Four very important clinical issues are discussed this month including inappropriate sharing of insulin pens, improper cleaning of glucometers between patients, and sharing of lancets or lancet holders.
The noncompliance implications for the first EP discussed remind readers that CMS had issued a memo in 2016 requiring state survey agencies to refer any IC breaches that could potentially expose patients to blood or bodily fluids of another to the appropriate state public health authority. TJC in the guidance advises its surveyors to contact the Standards Interpretation Group for an “escalation evaluation.” We will be extra blunt: the issues discussed in this column could lead to adverse determinations such as immediate jeopardy and preliminary denial of accreditation.
We have followed for 15 years the press announcements about hospitals where insulin pens were shared between patients and the adverse media attention and survey attention these organizations have received. That plus the deterioration of reputation that results should make all readers of our newsletter and this column convinced that similar situations will never be allowed to occur in your organization.
The discussion about glucometer cleaning and lancet use in the consistent interpretation column should lead readers to the same conclusion about prevention and adherence to the manufacturer’s instructions for cleaning glucometers. They also point out that some glucometers are approved by the FDA for single patient use and others are approved for multi-patient use.
Those that are approved for multi-patient use will have detailed instructions on how to clean the device between patients. You want to ensure that all staff using multi-patient use glucometers adhere to the IFU for cleaning and have the required cleaning agents recommended by the manufacturer.
We would encourage all readers to carefully review this month’s consistent interpretation column with hospital quality, infection prevention, nursing, and education staff to assess your own risks on these critically important issues.
 Sentinel Event Alert – Infusion Pumps:
Sentinel Event Alert – Infusion Pumps:
TJC issued Sentinel Event Alert #63 in April discussing safety strategies for use of smart infusion pumps. It contains valuable information from ISMP and ECRI as to the root causes of infusion pump errors, such as bypassing the integrated software, or not integrating the pumps electronically with your medication orders in the EMR. The software in the pump that contains the library of correct dosages and infusion rates, which many readers know as “guardrails,” now is described with a new acronym called DERS, or “dose error reduction software.”
As is customary, TJC provides recommended actions, and in this case eight. The first recommended action is to assign responsibility to a project team or department, such as your pharmacy and therapeutics committee, for smart infusion pump interoperability, developing and maintaining the DERS, changes to infusion protocols, and pump maintenance.
Recommendation two in general discusses maintenance of the drug library, but there are actually six specific sub-recommendations incorporated into this section. One of the ways in which we typically see hospitals maintaining their drug library is by obtaining management reports, or feedback on how many times the DERS is bypassed, and for which drugs.
TJC supplies guidance here from ISMP that monitoring should actually be in real time and alerts should be received when infusions are bypassing programmed dose limits. This is a very interesting recommendation in that you have an opportunity to potentially intervene in real time to prevent patient injury.
As with any Sentinel Event Alert, there is no mandate from TJC to implement all of the recommendations contained in the alert. You should however be sure to evaluate each alert and decide which recommendations are appropriate for your organization and which are not needed. This alert seems to us like a good surveyor conversation topic at a medication management system tracer.
You certainly would not want to be in a position of stating you have not seen the alert or have not considered the recommendations. As you start your analysis be sure to see if your radiology MRI area has an MRI compatible infusion pump. We sometimes see these, and at times there is no awareness that radiology has a unique infusion pump that is not part of the hospital wide update process.
Alternative Equipment Maintenance (AEM) Strategies:
The lead article in EC News is a lengthy discussion of alternative equipment maintenance strategies. It is very informative, and while AEM is acceptable to TJC and CMS, it is not a program we see many organizations choosing to implement. It requires excellent record keeping, literature review and risk assessment, and the potential that a future surveyor is going to disagree with your analysis. If you have the staff and resources and have implemented AEM already, then this article is a good opportunity to verify your program is compliant or fine tune it.
EC News contains an update from the FDA recommending that healthcare providers transition away from crisis capacity conservation strategies such as decontaminating disposable respirators for reuse. They basically advise that given the increased supplies now available such reprocessing should no longer be needed.
There is also a link to the OSHA guidance that was issued during the height of the pandemic in April 2020 that had discussed reprocessing of respirators. However, with increased supplies and FDA guidance to move away from reprocessing, we wanted to highlight the last paragraph from this OSHA memo.
“Citation guidance:
OSHA will, on a case-by-case basis, exercise enforcement discretion related to the reuse of FFRs that have been decontaminated using the methods recommended above when considering issuing citations under 29 CFR § 1910.134(d) and/or the equivalent respiratory protection provisions of other health standards in cases where:
- Other feasible measures, such as using partitions, restricting access, cohorting patients, or using other engineering controls, work practices, or administrative controls that reduce the need for respiratory protection, were implemented to protect employees;
- The employer has made a good faith effort to obtain other alternative FFRs, reusable elastomeric respirators, or PAPRs, including NIOSH-certified equipment or equipment that was previously NIOSH-certified but that has surpassed its manufacturer’s recommended shelf life (in accordance with OSHA’s April 3, 2020 memo), that is appropriate to protect workers;
- The employer has monitored its supply of FFRs, prioritized their use according to CDC guidance, and controlled the number of times a respirator is decontaminated before issuing a new one given supply level and burn rate considerations; and
- Surgical masks and eye protection (e.g., face shields, goggles) were provided as an interim measure to protect against splashes and large droplets (note: surgical masks are not respirators and do not provide protection during aerosol-generating procedures).”
The importance of this guidance is that discretion is a two-way street. Discretion to not enforce or discretion to enforce. So, if you are still reprocessing, you may want to take a look at this EC News article and reconsider that decision.
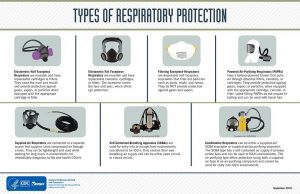
The terminology and description of the different types of respirators is sometimes confusing, so we have included here a CDC infographic that identifies the different types of equipment in use throughout the nation. View a larger depiction of the infographic here:
Conventional, Contingency, and Crisis Care Standards:
EC News has a thought-provoking article on implementing “Conventional, Contingency and Crisis Care Standards” that should be shared with your EM team and considered when you do revisions to your plan. Planning for an influx or surge has been a feature of the IC and EM standards for many years. Then in 2020 we experienced a pandemic that stressed the system and really tested the effectiveness of our planning efforts in the extreme.
This article points out that the National Academy of Medicine has recommended EM planning to three levels: conventional, contingency, and now crisis. During 2020, there were shortages of the previously discussed staff respirators, ventilators, and oxygen. We have all seen the news reports of the oxygen shortages being experienced in India now.
The EC News article provides a link to a January 2021 memo from Johns Hopkins Bloomberg School of Public Health that discusses oxygen conservation strategies and techniques to prevent mechanical breakdowns in your supply system.
Crisis care planning is not yet a requirement of the standards, but we have read that TJC will be revising the standards in the near future. As you critique the effectiveness of the past years’ experience and refine your EOP you may want to consider this suggestion.
Medical Gas Room Signage:
The last issue we want to discuss from the May EC News is the article on Medical Gas Room Signage. This is a point of confusion as the requirements TJC or CMS apply differ based on the gas supply system present and the types and amount of gases stored. Remembering which sign is required in different situations is difficult.
This article explains the requirements better than just reading the standards and more importantly they include a decision tree or flow chart that depicts the signage required for each situation. We suggest that their flow chart be discussed and analyzed at an environment of care meeting and used during EC or Quality rounds to verify that you have the correct signage present.

COVID-19 Test Positivity Rates:
The last two months we provided the link to the data CMS is analyzing relative to Covid-19 test positivity in counties throughout the US. CMS and Joint Commission have been examining this data to determine suitability for survey. We have reproduced that link again for your use.
https://data.cms.gov/stories/s/q5r5-gjyu
The bad news is we see some slippage in end of April data with more red and yellow counties, and fewer green counties.
2/24/21 3/23/21 4/27/21
Green 1327 Green 1892 Green 1795
Yellow 1541 Yellow 1154 Yellow 1209
Red 337 Red 113 Red 204
Interoperability Requirements:
As mentioned earlier in this issue, CMS issued QSO 21-18 on May 7th, 2021 providing an advance copy of the interpretive guidance for their interoperability requirements for both hospitals and critical access hospitals. The memo indicates that the requirements will become effective as of June 30, 2021. The QSO memo makes it clear that hospitals and critical access hospitals have to send notice to other providers for emergency room visits and admissions, external transfers, and discharges.
The first CMS tag touched is A-0470 and it requires notice be sent for registration as an inpatient or emergency room patient to external providers. CMS points out that this may require two notices, one stating that the patient has registered for treatment in the ED, and a second notice stating the patient has been admitted to the hospital. CMS also makes it clear in their guidance that emergency room notice must be sent regardless of the decision to admit or not.
The second tag addressed is A-0471 and it requires notice be sent to post-acute providers when a patient is discharged from the hospital.
The third tag addressed is A-1673 which contains the same registration in the ED or as an inpatient notice be sent but the guidance specifically refers to psychiatric hospitals. In this case, a specific consent must be obtained from the patient to send the notice to other providers. This contrasts with the general hospital guidance which included obtuse language stating the notice sent should “not be inconsistent with the patients expressed privacy preferences.”
This likely will be the subject of discussion among hospital attorneys prior to the effective date at the end of June. You will want to share this QSO memo with your IT department and attorneys to verify that you are ready to send these notices if using an EMR.

Consultant Corner
Dear Readers,
We hope that you have all gotten a chance to check out our NEW WEBSITE to view all the new and reformatted tools available to you! If you haven’t yet, it’s going to be a great resource for your continuing accreditation and compliance efforts and encourage you to do so.
With word getting out that surveys are up-and-running, there is extreme demand for accrediting expertise. Please contact us soon! We can help you overcome the year-of-the-pandemic and support your preparation for survey.
Jennifer Cowel, RN MHSA
JenCowel@PattonHC.com
Kurt Patton, MS RPh
Kurt@PattonHC.com
John Rosing, MHA
JohnRosing@PattonHC.com
Mary Cesare-Murphy, PhD
MCM@PattonHC.com
