Question:
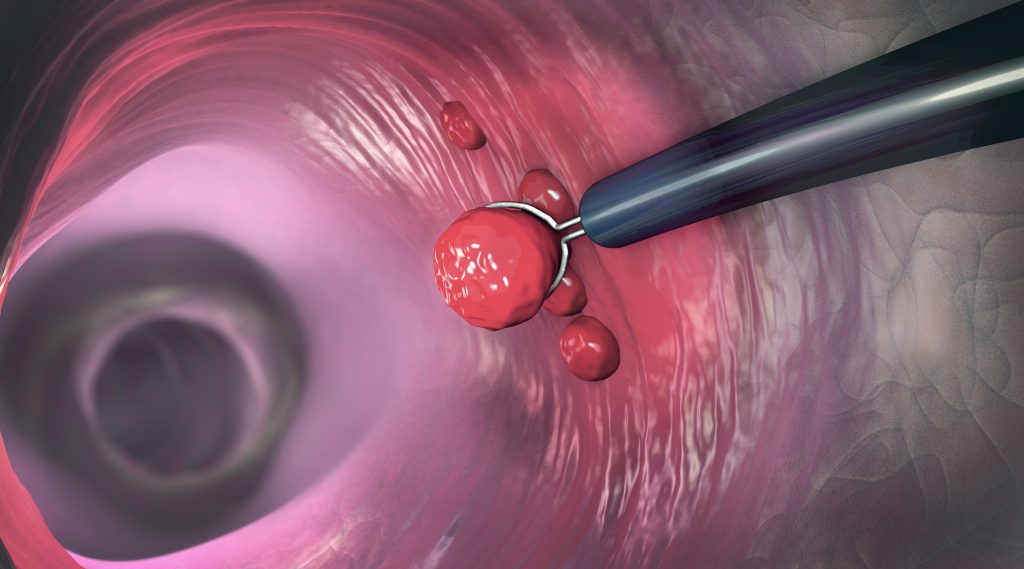
I was rounding in our Endo Department and in one of the charts we reviewed, the patient signed a consent for a colonoscopy and the post procedure note included removal of polyps. Does polypectomy and biopsy not need to be specifically mentioned in the consent as long as it is discussed as a risk?
Would this be a finding during survey? We were wondering how explicit these consents need to be because sometimes an intervention is added due to findings.
Answer:
CMS expects the consent form to, at a minimum, “name the specific procedure for which consent is being given.” If a component of a multi-component procedure is unanticipated, we do not believe there would be any penalty.
If, however, removal of a polyp for biopsy is a routine and anticipated part of many colonoscopies, we would recommend the addition of the phrase “possible removal of polyps” be included on the consent form. “Colonoscopy with possible removal of polyp(s)” would be best, most accurate practice.

Leave a Reply