November 2022
Inside This Issue
New ORYX Performance Measure Requirements for 2023:

The November issue of Perspectives is quite brief, with no new standards announced, but with several important pieces of information to help prepare for the coming year.
The lead article discusses the 2023 ORYX performance measure requirements and there are three new electronic quality measures available for potential use in 2023: severe hypoglycemia (HH-01), severe hyperglycemia (HH-02) and ST-segment elevation for MI patients in the ED (OP-40).
The requirement is to use four electronic clinical quality measures for four quarters in 2023. In 2022 TJC had permitted optional measures for perinatal quality, cesarean birth (PC-02) and severe obstetric complications (PC-07) to fulfill its ORYX requirements and these measures will still be used in 2023 for CMS and TJC.
New Safety Briefing for 2023 Surveys: 
TJC also announced a new survey process issue they call a “safety briefing” for all surveys beginning in 2023.
This is not a tracer, but rather a briefing you will provide to surveyors as part of the opening activities to help guide them in the event of a local emergency, workplace violence issue, or any civil unrest or labor actions that may be taking place during the survey.
This is intended to be five (5) minutes or less, just enough to guide the surveyors on what they are expected to do in the event something happens while they are onsite.
As it reads, it sounds to us like a content point you may already have depicted in some portion of an employee orientation. But you will want to figure out what concise content or guidance you will want to provide to your surveyors.
In addition, the issues may change throughout the year as activities happen in your community, but the actions you want your surveyors to take may remain consistent.
2023 Standards Database and Updates: 
Perspectives also announces the pending release of the 2023 manuals and updates. Print copies are expected to be released by the time you are reading this newsletter, and more importantly we noticed that the E-edition already has the 2023 standards database available.
High-Risk Medical Equipment Preventative Maintenance:
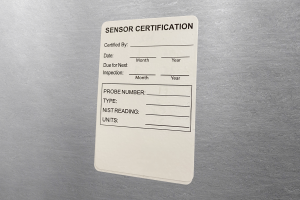
This month’s Consistent Interpretation column is brief, discussing EC.02.04.03, EP 2, the inspection, maintenance and testing of high-risk medical equipment. TJC reports that this is scored in just under 10% of hospital surveys. The challenge here is the inspection requirement is 100%. That means that even one piece of expired high-risk medical equipment is scoreable.
The guidance/interpretation section is more geared to advising surveyors about the specific standard to score different issues rather than guidance on how to be successful. We do see high-risk medical equipment fairly often on consultation surveys, where the inspection sticker is either expired or missing.
In theory your hospital biomedical department or vendor should be looking for such high-risk equipment prior to expiration and be completing the inspection for the coming timeframe, however as we all know, sometimes this equipment, often on wheels, or easily carried goes missing from the area to which it was assigned.
Another problem which can occur is a department purchases a new piece of high-risk medical equipment and it gets delivered directly to the ordering department, bypassing biomed. There are two potential actions to consider here:
- The first is to train clinical staff when using any high-risk medical equipment to look for the inspection sticker and date, to verify the equipment is up to date and safe to use in patient care. If it is not, the device should be sequestered, biomed called and the device not used until the inspection is completed.
- A second activity to consider is if any new medical equipment is delivered directly to the ordering department to call biomed before placing that new device into service. The equipment must be added to the medical equipment inventory, the MIFU analyzed to determine inspection requirements/frequency and an initial inspection be completed before use.
Again, if staff is trained to look for the inspection sticker and dates for medical equipment inspections before use, any failure to get the new item inspected should be stopped by this clinician verification. As there is no master list of what equipment should be categorized as “high-risk,” the article is useful in providing a few examples “to include but not limited to” on your list.
New TJC FAQ on Healthcare Worker Masking: 
Last month we discussed the CDC’s latest guidance on masking for healthcare workers. TJC has now issued an FAQ on the subject where they state they expect healthcare organizations to develop policies and procedures on masking that are consistent with that CDC guidance, as well as any applicable state regulations.
TJC also mentions in this FAQ that their surveyors will be wearing masks while visiting your organization, and they ask that staff of the organization also wear masks while present with the surveyors.
Most Problematic EC/LS Standards and EPs:
Last month TJC conducted its annual Executive Briefings presentation, where their program and content experts present on the most difficult standards and new directions the company may be taking.
This month’s EC News has a brief summary of Herman McKenzie’s presentation on the five most problematic EC/LS standards and elements of performance. These are in rank order:
- EC.02.06.01, EP 1: Interior spaces are safe and suitable
- LS.02.01.35, EP 4: Nothing should be touching sprinkler pipe above the ceiling
- EC.02.05.01, EP 9: Label utility shut down controls
- EC.02.05.05, EP 6: Inspect and maintain non-high-risk utility system components
- LS.02.01.10, EP 14: Seal the space around pipes, etc., with fire rated material
The article provides insight on how the surveyors go about finding these standards noncompliant and the types of problems that are noticed.
The first problematic standard we have talked about many times before in this newsletter as just about any defect in the environment can be scored against this EP. TJC mentions stained ceiling tiles as one example and nurse call cords in the bathrooms that are wrapped around the grab bar, and left unreachable from the floor.
 The challenge is to be able to identify these problems yourself ahead of survey and get them corrected. Having a good internal inspection process, looking for these issues as well as torn or broken furniture, torn stretchers, damaged flooring or anything that looks risky from an environmental perspective.
The challenge is to be able to identify these problems yourself ahead of survey and get them corrected. Having a good internal inspection process, looking for these issues as well as torn or broken furniture, torn stretchers, damaged flooring or anything that looks risky from an environmental perspective.
Sprinkler piping being used to help support other materials above the ceiling is the second most problematic standard. The term “support” is used loosely as in reality anything touching that sprinkler pipe is likely to be scored noncompliant. We see this often on consults and on official TJC survey reports and many times it is noted as observed and corrected on site. This makes it seem as if it is easy to fix, but if it is already been noticed by the surveyor, it really is too late.
TJC recommends educating any staff or contractors who may be working above the ceiling that nothing can be resting on or attached to the sprinkler pipe. Better still is after any above the ceiling work is done an inspection should take place at completion to verify the staff or contractor did not violate the guidance you provided them.
 The third most frequently scored standard discussed is utility system controls needing to be properly labeled. Here TJC provides insight on how surveys find this noncompliance by opening electrical breaker boxes and looking for any “spare,” unlabeled breakers that might be in the on position. If the spare, unlabeled breaker is on, chances are it is actually providing current to some part of the hospital or equipment. Thus, the organization has failed to properly label its utility shut offs.
The third most frequently scored standard discussed is utility system controls needing to be properly labeled. Here TJC provides insight on how surveys find this noncompliance by opening electrical breaker boxes and looking for any “spare,” unlabeled breakers that might be in the on position. If the spare, unlabeled breaker is on, chances are it is actually providing current to some part of the hospital or equipment. Thus, the organization has failed to properly label its utility shut offs.
 The fourth most frequently scored issue is inspection, testing and maintenance of non-high risk utility system components. Again, TJC shares one method surveyors have to detect noncompliance and this is storing anything within 3 feet of the breaker box, thereby blocking access. In other words, not maintaining the utility system components. We have used pictures in many of our educational programs to help draw attention to this issue of the kinds of materials that get parked in front of breaker boxes, often right in front of the “Do Not Block” sign.
The fourth most frequently scored issue is inspection, testing and maintenance of non-high risk utility system components. Again, TJC shares one method surveyors have to detect noncompliance and this is storing anything within 3 feet of the breaker box, thereby blocking access. In other words, not maintaining the utility system components. We have used pictures in many of our educational programs to help draw attention to this issue of the kinds of materials that get parked in front of breaker boxes, often right in front of the “Do Not Block” sign.
 The fifth most frequently scored issue was sealing the penetrations around pipes and cables going through walls. Prevention here is similar to the discussion on sprinkler pipes. Staff performing the above the ceiling work need to be educated on the need to seal these gaps and again an inspection process after the work to verify the work was done in a compliant fashion.
The fifth most frequently scored issue was sealing the penetrations around pipes and cables going through walls. Prevention here is similar to the discussion on sprinkler pipes. Staff performing the above the ceiling work need to be educated on the need to seal these gaps and again an inspection process after the work to verify the work was done in a compliant fashion.
 Managing an Evacuation and Lessons Learned:
Managing an Evacuation and Lessons Learned:
EC News has an article prepared by the Avista Adventist Hospital in Colorado, describing their actual evacuation of their facility due to an area fire that filled the hospital with smoke. They describe completing their evacuation in two hours and some of the lessons learned from their actual experience.
 One such example is the difficulty they experienced in being able to access electronic medical records in the transfer facility and the subsequent work they have done to make this easier if there is a “next time” this has to be done. This article should be shared with your EM team for analysis of your own evacuation planning, should that ever be needed.
One such example is the difficulty they experienced in being able to access electronic medical records in the transfer facility and the subsequent work they have done to make this easier if there is a “next time” this has to be done. This article should be shared with your EM team for analysis of your own evacuation planning, should that ever be needed.
Covid Vaccination Requirements of the Workforce: 
CMS has one new QSO memo of importance to our readers concerning Covid vaccination of the workforce. This is QSO-23-02 and it replaces the earlier QSO-22-07, QSO-22-09 and QSO 22-11 discussing vaccination requirements and survey scoring. Like the predecessor memos, this one has a series of attachments for providers of all types. The hospital memo is again attachment D.
There is some good news here that the changes discussed should not be labor intensive. CMS is really only changing the types of surveys where this review of vaccination data should take place and how they score the findings. They did not change the basic requirements for what constitutes complete vaccination.
The first change is that CMS expects vaccination data to be evaluated on full initial and recertification surveys, as well as complaint surveys where vaccination is at the core of the complaint. The routine complaint survey on issues such as patient rights or grievances do not require examination of the vaccination data, however the survey team could decide to look at it if something arises during their survey.
The second change is in the scoring, described in the attachment for the provider type. For hospitals they define egregious noncompliance as less than 50% compliance and/or 1 or more missing policies for the staff vaccination program and this would be scored at a COP level. A lesser level of noncompliance would be scored at a standard level. Be careful if you try to print this entire memo as with all the attachments it exceeds 160 pages. All you really need is the 5-page QSO memo and your provider type attachment.
Chapter 797 Has Officially Been Published: 
The USP has just announced on November 1st that the new version of Chapter 797 has been published. This will become the official requirement for sterile compounding in November 2023. One likely change, that may take a lot of planning and preparation, is the anticipated monthly surface sampling in all classified spaces, rather than today’s twice-yearly sampling. Contracting this task out to a vendor may be very costly, if the vendor even has the capacity to expand to monthly service for all of their clients. Taking on the task internally will require extensive preparation including competency validation, purchase of incubators, space to perform incubation etc. A year seems like sufficient time to prepare, but our advice is to start that planning now as there are many logistical issues to be evaluated in order to be able to start monthly surface sampling on time.
Consultant Corner
Dear Readers,
November is a month for thanks giving, and we would like to thank you, our readers. We hope you have a great month!
Jennifer Cowel, RN MHSA
JenCowel@PattonHC.com
Kurt Patton, MS RPh
Kurt@PattonHC.com
John Rosing, MHA
JohnRosing@PattonHC.com
Mary Cesare-Murphy, PhD
MCM@PattonHC.com
